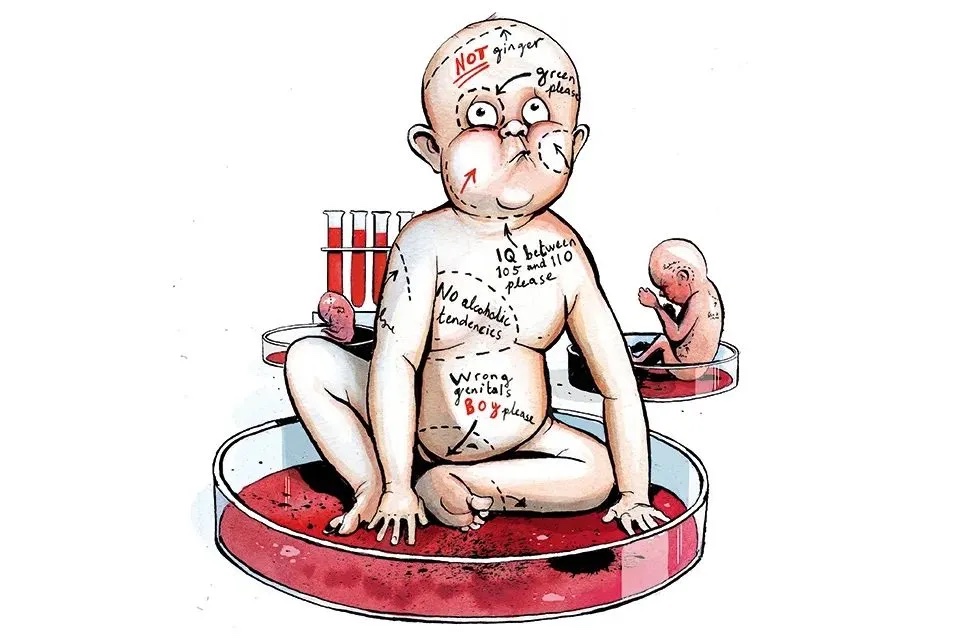
I have decided to divorce my wife after 31 years on scientific grounds. Though perfectly happy, on reassessing my original decision to enter matrimony it has emerged that at no point was that choice subject to peer review, there was no randomized control trial, the experiment could not be replicated and the data-set on which I based my decision failed to provide the levels of statistical confidence required.
I don’t think my decision to marry was bad, but it was definitely unscientific. Most important decisions are. Indeed if one phrase has most irritated me in the past few months, it is ‘the science’. What is ‘the science’ on masks? The implicit assumption is that we can only act on generalizable, definitive facts. This is unsafe in the instance of COVID, since a combination of medical ethics and short timescales means we still don’t know most of what we need to know in order to develop nuanced models and reliable recommendations. Science’s arbitrary p-value obsession also runs counter to real-world decision-making, where trade-offs must be made between the reliability of information and the consequences of acting on it. If business demanded scientific levels of certainty in decision-making, the economy would collapse. There is no Isaac Newton for ‘Should I open a Turkish restaurant in Hoboken?’ because, in reality, what you don’t know is always more critical than what you do.
***
Get a print and digital subscription to The Spectator.
Try a month free, then just $7.99 a month
***
Let’s take face masks. One thing we don’t seem to know is the path dependency of COVID-19. In particular we don’t know if the size of the initial viral dose has a bearing on the course or severity of the disease. Most models appear to assume that infection is a binary matter. But if this is wrong, it is possible masks may do double duty by not only reducing the rate of cross infection but also improving outcomes — and even the rate of onward transmission — among those infected.
The strange thing is that almost every doctor I speak to believes that, yes, the level of the virus’s initial dose will affect the outcome of the disease. But because the science cannot be established (the experiments required would be unethical), no one can proceed on the basis of this possibility. That is a pity, since it could lead to new approaches to prevention and treatment, for instance in the area of ventilation and fresh air. Before air conditioning, hospitals were routinely designed with high ceilings and large, opening windows as a matter of course to reduce the concentration of pathogens. Spanish flu was treated successfully in outdoor hospitals. One cultural difference worth exploring is that Germans sleep with their windows open (the Teutonic world is the cultural opposite of France, where it is believed that anyone sitting in a draught for ten minutes will soon die a horrible death). The miasma theory of infection might have been scientifically wrong, but it may have led to beneficial design behaviors.
I’m not anti-science. My brother is an astrophysicist. This means that he knows a huge amount about galaxy formation, but if you put him in a branch of Ikea and told him not to come home until he’d chosen a sofa, he’d starve to death there, having failed to determine a robust algorithm for furniture selection. An insistence on the scientific method has costs as well as benefits — it is slow and may reduce the solution to those actions you can easily quantify or justify in advance. There is, after all, a good reason why humans have evolved decidedly unscientific instincts for decision-making: in the messy world we inhabit, the facts that are available are usually not important, and the facts that are important are usually not available.
This article was originally published in The Spectator’s UK magazine. Subscribe to the US edition here.