When COVID-19 vaccines arrive, are people going to agree to have them? Most of the world’s advanced economies have chosen to suppress the circulation of the COVID virus, SARS-CoV-2, by lockdown, to great economic and social cost. And each of these national choices has been predicated on the assumption that the vaccines now under development will soon be available, will be protective, and will by their general distribution prevent further circulation of the virus. A further assumption is that the negative effects of lockdown can be accommodated till then. So where are we after six months of lockdown and social distancing?
Scientific groups worldwide have now taken COVID-19 vaccines beyond the first developmental phase including at least one vaccine intended for single-dose use; and huge investment has been committed to bringing any proven vaccine quickly on stream. Data from published vaccine trials has been encouraging (even if the Oxford vaccine was paused this week after a volunteer suffered an adverse reaction), but it has mostly concerned recipients who are less than 50 years old and fit, i.e. not those at special risk from COVID-19. Future vaccines will have to confer protection from illness on those who are at risk of serious morbidity due to advanced age, obesity or underlying illness.
In the second phase of vaccine development, safety and efficacy in the presence of circulating SARS-2 virus is being examined. Adequate vaccines against several coronaviruses of farm animals and poultry already exist, but for a human COVID-19 vaccine a high degree of protection will be expected and it will be the minimum criteria that there is no infectivity following exposure.
When satisfactory COVID-19 vaccines do become available, perhaps as early as next year, personal protection from infection will be the primary motive of their willing recipients. But globally the aim of vaccination must be much more ambitious: irreversible elimination from human circulation of SARS-2 virus. It is as yet unknowable whether the level of vaccine acceptance attained will allow this to happen. Will more than 90 percent population coverage be required, or will less suffice? Will the effect of COVID-19 vaccines in mitigating illness among the most vulnerable eliminate the super-spreading phenomenon that has until now produced crops of new cases?
Healthcare workers urgently need vaccine protection both for their own sakes and because it will relieve them of the encumbrance of protective equipment. Can their vaccination be followed by a reliable demonstration of acquired immunity and allow them to deliver the routine health services that have been compromised by attention given to COVID-19?
Licensing of COVID-19 vaccines can be fast-tracked with derogations wherever possible, but not to the extent of tolerating products that only ever confer partial or short-lived protection from illness. Nor will vaccines alone be the ‘get out of jail’ card. Eliminating human viruses is not rapid or straightforward as was learnt during the eradication of smallpox in the 1960s and 1970s, and again today in respect of polioviruses.
***
Get a digital subscription to The Spectator.
Try a month free, then just $3.99 a month
***
Furthermore, SARS-2 is the third zoonotic coronavirus to have spread to humans within two decades. It was possible to interrupt circulation of SARS and MERS as soon as obstacles were put in their way but this has been impossible for SARS-2 which may continue to find ways of persisting among humans. Whether it can be stamped out, and in much shorter order than the previous two, remains questionable. To get SARS-2 under control now requires not just vaccines but urgent consideration of their global use, and this should be uppermost in the thoughts of public health strategists. A campaign to promote vaccine acceptance cannot start soon enough, and well-judged public education initiatives will be needed. There have been opponents of vaccination since Edward Jenner created the smallpox vaccine, and their notions continue to have widespread currency both in the developed and the developing world.
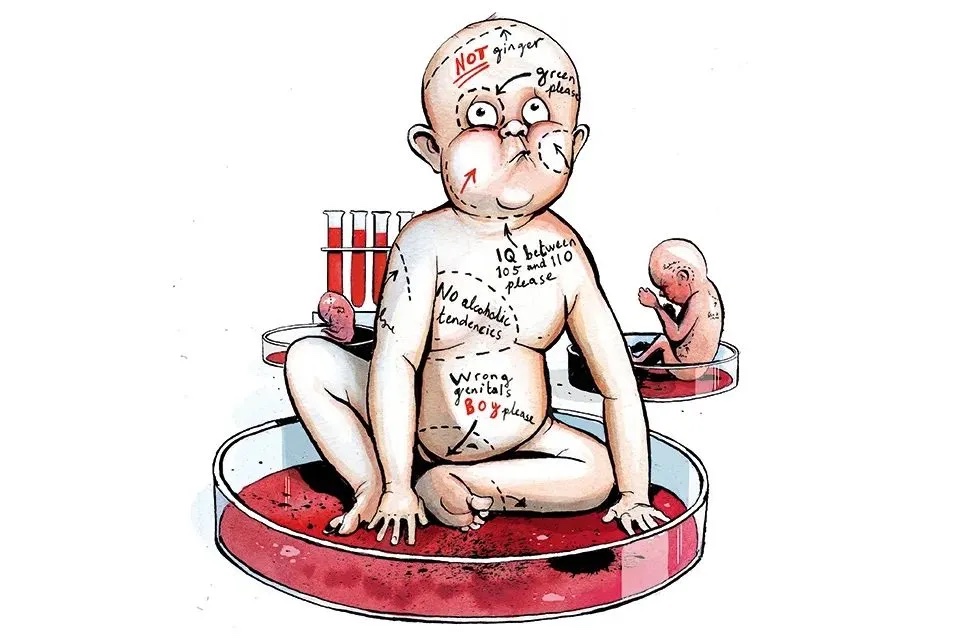
In particular, opposition to mass vaccination can be expected against an illness so largely confined to mature adults, and social media will weaponize the argument that children, being virtually unaffected by COVID-19, do not need to be immunized (the best counter-argument to this will be that it reinforces their right to go to school which has repeatedly been denied them). People who have been ill and declare themselves immune to SARS-2 virus may also not wish to be vaccinated, but present antibody tests are inadequate to tell whether or not they are justified in thinking so. Others will simply refuse the vaccine. Mere slogans such as ‘do it for grandma’ are unlikely to win them over.
It is conceivable that the infectivity of SARS-2 virus will remit spontaneously, but it is more likely that it will linger rather as, historically, successive new influenza strains did in 1889-91, 1918-9, 1957 and 1968-9. In the case of SARS-2 virus only universal vaccine uptake is sure to make it go away, and this in turn presupposes that safe and effective vaccines will be abundant, inexpensive and deliverable, and that the case for receiving them will have successfully been made. The world order that after a long struggle saw off smallpox is surely not going to squander the chance to remove SARS-2 virus from human circulation, but the challenge is a global one that demands international funding and co-operation. It won’t be easy to meet, and it may take some time.
Dr Philip Mortimer is a former director of Britain’s Public Health Laboratory Service and the Sexually Transmitted and Blood Borne Viruses Laboratory. This article was originally published on The Spectator’s UK website.