‘Where are you now?’ I ask John. On the screen, I see him seated on a stained orange couch, beanie pulled low over his forehead. He looks a little sleepy, an effect of the heroin he used before calling me.
‘At my buddy Nick’s — he’s letting me stay on his couch.’ Someone starts rapping in the background. Then someone yells at him, and the rapper yells something back, and then laughter. John looks off in the direction of the sound, ‘Shut the fuck up! This is an important call.’
I am a physician who specializes in the treatment of addiction. John came to me seeking a prescription for buprenorphine, a life-saving medication that alleviates opioid withdrawal, decreases illicit drug use, and has a clear mortality benefit. Before the COVID-19 pandemic was declared a national emergency, federal regulations mandated I see every patient in person before I could prescribe buprenorphine. Under the declaration, this requirement has been waived. I can prescribe to patients I see virtually or, if they don’t have access to a smart phone or tablet, I can simply prescribe over the phone.
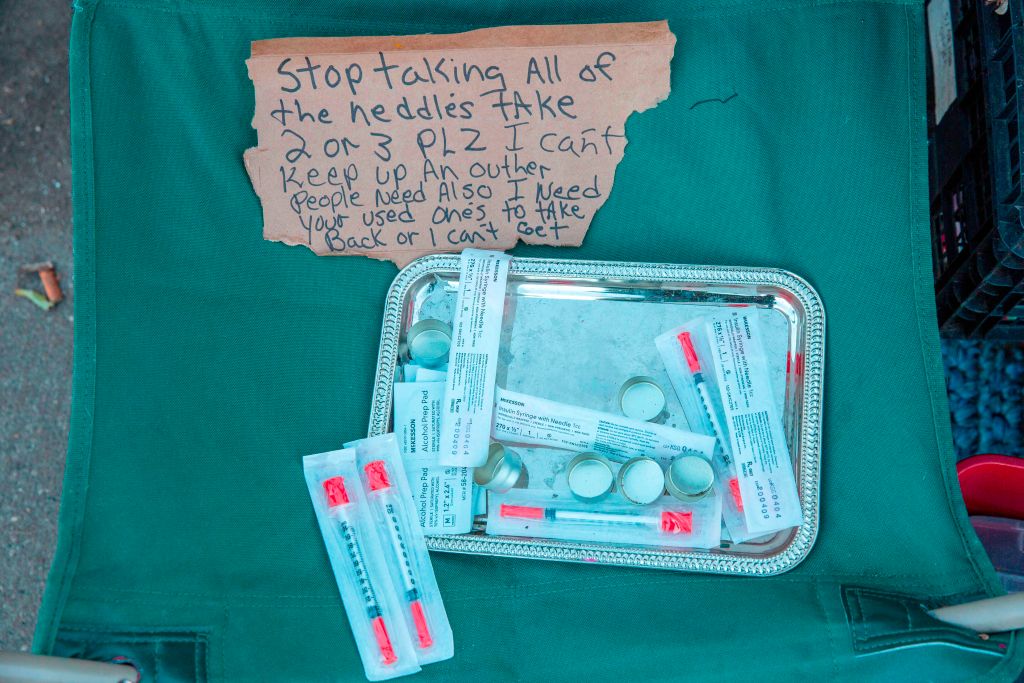
The rules were revised in order to promote physical distancing, and thus decrease the spread of COVID-19. But the change has also profoundly improved the ability for providers like me to address the ongoing national epidemic of addiction and overdose that preceded COVID-19, and that will almost certainly outlast it. Many of my patients are unemployed, tenuously housed, or without any housing at all. With this rule change, I can now prescribe to patients who don’t have bus money to make it to clinic, but who have a phone, or can borrow one. I can prescribe to patients I would never see in clinic, even if I gave them bus tickets, because it is too hard to navigate our halls and elevators while also carrying their sleeping bags and tents. And I can see patients who live in rural parts of our state and don’t have the resources to travel. Certainly, there are still significant barriers to care — access to phones, wireless, and data plans chief among them. Nevertheless, this is a critical advance.
Providing care virtually also has another important benefit. In the rush of a busy clinic day, it can be difficult to remember to ask about the details of a patient’s life, the context in which their health, disease, and habits develop and thrive. It is even harder to pay sufficient, focused, attention to the answers. But when I see John on screen, I don’t have to remember to ask if he smokes. He’s puffing away in front of me. More than that, I see the relief it brings him, on that orange couch, in this scary time, and that helps me understand when he says he’s not yet ready to quit. When I see my next patient, I don’t need to remember to inquire about housing: he’s calling from a Walmart parking lot, near where he plans to camp for the night. Later that evening, I see only the shadow of my last patient, inside her car, tight and dark. I don’t need to wonder why her answers are clipped, and she can’t seem to focus.
Seeing my patients like this does not mean I now understand what it’s like to be without shelter, or that I get what it is like sleep in my car, grateful for slim protection of doors that lock. I have the great fortune of talking to patients from my warm office. When we finish, I have a home to return to. But at the very least, I am denied the luxury of tucking my patient’s lack of shelter, or loneliness, or nighttime fear into the corner of my mind as an abstraction.
Talking to John, I can see a stain in the shape of Florida snaking behind him on the couch. I can also see the affection on his face when the rapper starts up again. He smiles and shakes his head, ‘Man, he is terrible.’ He calls out, with renewed force, but no anger: ‘I said, shut the fuck up!’ Then he moves into the bathroom to sit on the edge of the tub to finish our conversation. That is another gift of this technology: I see John’s resilience, and know he is not entirely alone.
COVID-19 has steeped our country in sorrow, fear, and isolation, the perfect soil for addiction to take root. My clinic has already seen a surge in patients seeking care for substance use disorders, and demand for our services will likely remain high, or grow. There have been so few silver linings to this horror: maybe the air is cleaner, maybe we are a little less rushed, maybe we’ve learned that not all meetings require a drive across town, or a flight across the country. This little rule change with its life-saving effects is another bit of silver. I can take care of patients in need of addiction services, wherever they are, whenever they are ready. When the world goes back to normal, or whatever version of normal is possible, it is critical that the rule change remain in place, a tiny, shiny, nugget of hope.
Dr Jessica Gregg is associate professor of medicine at Oregon Health and Science University, medical director for the OHSU Addiction Medicine ECHO clinic and associate program director for the OHSU Addiction Medicine Fellowship.