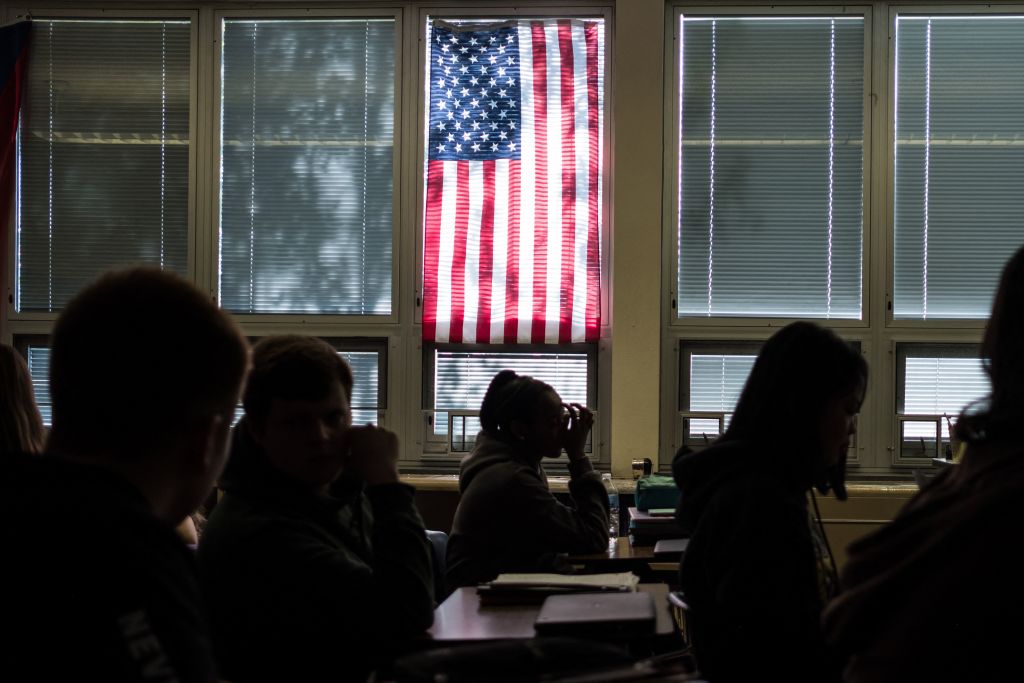
How well-equipped are we to beat back COVID-19? With the US passing 200,000 deaths and infection rates once again soaring in Europe, there is seemingly no good news in sight. But what if it turns out human immune systems are better prepared to combat the novel coronavirus than we first assumed?
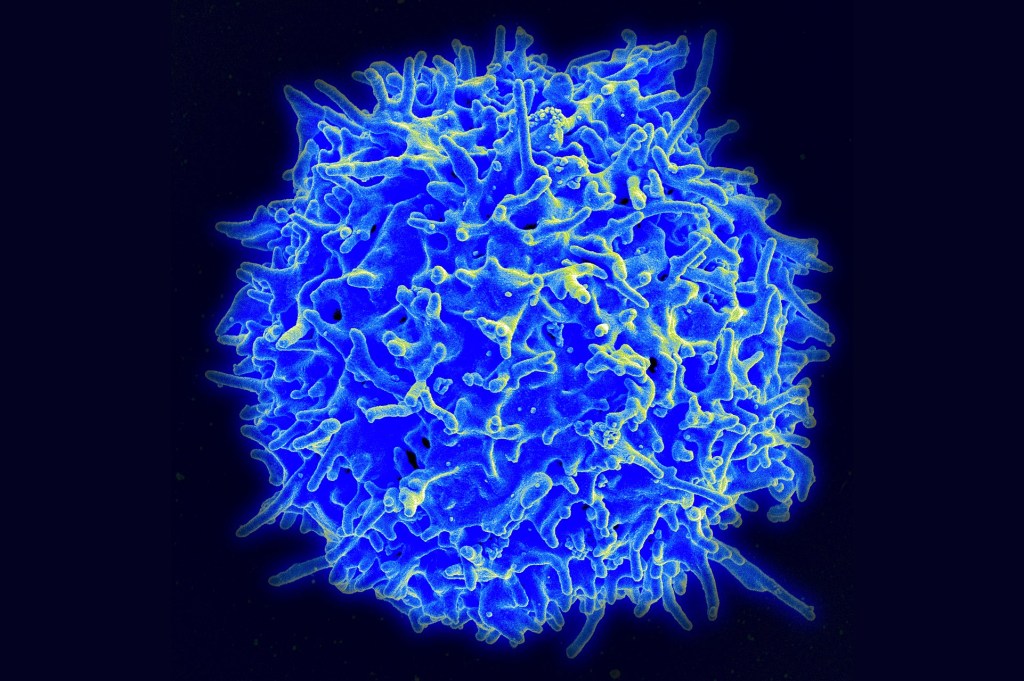
Drs Alessandro Sette and Shane Crotty of the La Jolla Institute of Immunology in California are behind several of the most significant studies of SARS-CoV-2 thus far. Their research into T-cells and their function in the immune system’s fight against the virus could play a pivotal role, in both the development of a vaccine and the possibility of attaining herd immunity against COVID-19.
The two immunologists explained their findings over a Zoom call with The Spectator last week.
Matt McDonald: Could you, in a nutshell, summarize what the major findings of your studies this summer were?
Alessandro Sette: So the first one was really early on…this was the first time where anybody had measured T cell responses to SARS-CoV-2. Basically, there are three parts of the adaptive immune system. One is the antibodies: the antibodies find the virus and neutralize it. So they’re very good to prevent infection. Then there are two types of T cells: the killer T cells and the helper T cells. Predictably, the function of killer T cells is to kill infected cells. This is important because once the virus is inside, the cell is no longer accessible for antibodies. The helper T cells help and they help preside over antibody generation, also killer T cells. Without helper T cells, you don’t get a good antibody response. It’s weak, transient, not strong in neutralizing, so they’re really important.
People were measuring SARS-CoV-2 antibodies, but nobody knew how to measure T cells. We developed the reagents to be able to measure both helper and killer T cells. Our goal was to measure immune responses in convalescent cases from not very severe COVID-19 cases. These were success stories: an image of what that would look like in terms of an immune response that wins over the virus.
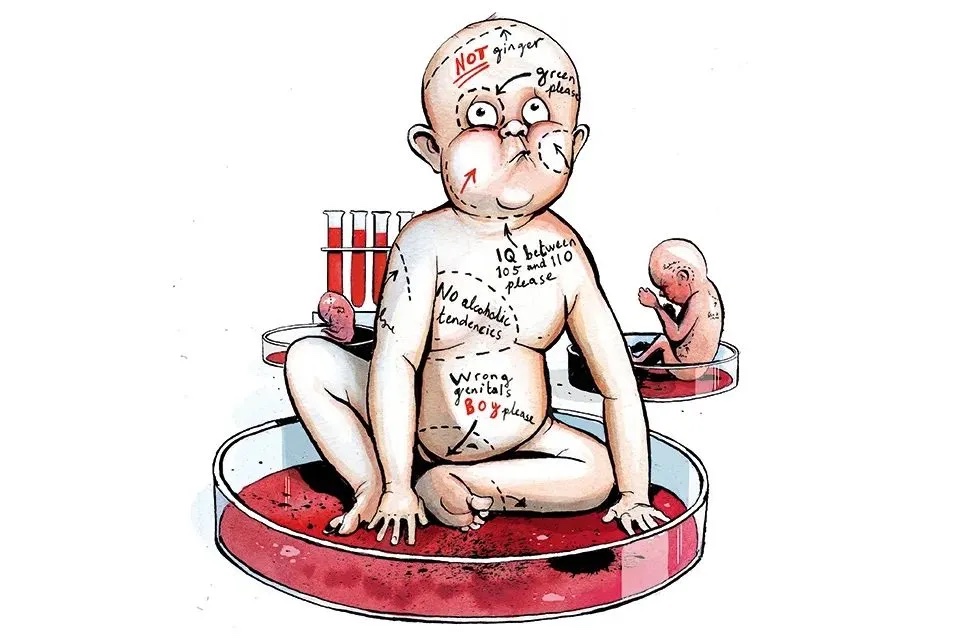
Then we looked at one of the targets of an immune response. Everybody’s working on vaccines based on spike [the sharp extensions on the outside of the virus which are important in the virus’ ability to stick to human cells] because it’s a good target for antibody responses. So we were able to answer: is spike also a good target for helper and killer T cell responses?’ And the answer was yes. So that was good news.
MM: There are several vaccines in development right now — Moderna, Pfizer-Biotech, Johnson & Johnson, Oxford-AstraZeneca. Oxford-AstraZeneca is using your findings — are the others, or are their approaches different?
Shane Crotty: The AstraZeneca and J&J vaccines work by triggering all three branches of an adaptive immune system: the killer T cells, the helper T cells and the antibodies. The RNA vaccines — being developed by Moderna and Pfizer — work by essentially infecting or getting inside cells and priming the killer T cells, helper T cells as well as antibody response. Most of their data indicates RNA vaccines do better with getting the helper T cell response than a killer T cell response. Then there is the protein vaccine approach, used by the Novavax vaccine, which is, I think in Phase Two right now. That elicits antibodies and helper T cells but not killer T cells.
MM: The biggest question arising from your studies is, how would you measure herd immunity? Does the T cell response that you guys record, does that amount to immunity?
SC: That gets pretty complicated. There are two parts to it. Firstly, what is going on with T cell responses during a SARS-2 infection? There is the adaptive immune system and there is the innate immune system. And they are different. The adaptive immune system, which is what Alex and I have been talking about, is the part which can specifically recognize a new virus, and which actually makes antibodies against SARS-2, or flu for example. The innate immune system just recognizes a virus as ‘a virus’. So those are separate.
The big question is: why do you end up with a cytokine overreaction [an excessive response of the immune system]? Is the problem the adaptive immune system, the innate immune system or both? What’s good, what’s bad? Our data indicate that the adaptive immune system works well. For any virus today to infect you, it has to have some sort of immune evasion strategy, otherwise you wouldn’t get infected. A lot of people have indicated this coronavirus is quite good at evading the initial innate immune response, which includes type one interferons. You don’t get an adaptive immune response until after you get an innate response. It is basically like the burglar alarm going off. It’s not until that alarm goes off that you can start getting a specific T cell and antivirus response. The longer the virus can hide from that innate immune response, the longer the virus delays the person being able to start making an antibody and T cell response. If you get that innate immune response pretty quick, on the other hand, then you get your adaptive immune response quick and you might have just an asymptomatic infection. Two papers that came out in Science yesterday really corroborate that pretty nicely. They pointed to the innate immune system as the problem in COVID-19.
MM: Why does the risk of developing severe symptoms increase with age?
AS: Your immune system has a pool of cells which are called naive cells, which are the ones that the immune system uses to develop a response against something that they’ve never seen. As you age, your pool of naive cells shrinks progressively. If you look at different people of the same age, some may have a larger pool and some a smaller pool. There’s that old cartoon that says that you can’t teach an old dog new tricks, which is one way to say that it’s difficult for an old immune system to recognize new viruses.
SC: The adaptive immune system has these three branches for a reason and it’s really like three branches of the military. They have different things that they’re good at. Your best case scenario is that you have so much neutralizing antibody that when somebody who’s infected coughs on you, you don’t get infected. Antibodies are the only thing that can do that. They can stop the virus before you have any cells that are infected. If, however, the virus gets past that and you have this infection in your nose and throat, T cells can recognize infected cells. The virus has to infect cells and T cells can tell that the virus is there. It’s the T cells, generally not the antibodies, that can kill off infected cells. So if the virus gets past the antibodies, you really want to have the T cells so that they can mop up. If you don’t have any T cells, you basically have to start from scratch. You may have to be sick for a week before you get the T cell response. The whole point of vaccines is so that you have the immune response before you get infected, so that your body has the head-start instead of the virus having the head-start.
From studying people with active COVID-19 infections, we think there is reasonable data indicating that if you don’t have antibodies but you do have T cells, then it is likely that the T cells would help control the virus. The question is, after the infection, how long does immune memory to SARS-2 last? But certainly our data point to T cells doing fantastic work, and as part of a vaccine they may be able to clear up infection that gets past antibodies.
MM: In the nine months that we’ve been dealing with this in this country, we’ve massively scaled up the ability to perform antibody tests. How big an operation would it be to do the same thing with testing for a T cell response?
SC: It’s at least 10 times harder and more expensive. The antibodies you can do with a tiny amount of blood as a biochemical assay and it’s stable, it doesn’t require a lot of storage. With T cells, it’s live cells.
AS: The key difference is, to measure the antibodies you really just measure the serum or the plasma because that’s where the antibodies are. The proteins are stable, while T cells are alive and they are very finicky. You either would have to analyze them fresh and that requires appropriate culture systems. And if you want to freeze them, they need to be frozen and thawed with particular care. It’s a very complicated type of assay.
We and others have been looking into the possibilities of devising this type of whole-blood assay for SARS-2 T cells. But those are very much still in very much in the drawing board stage.
SC: There is another story here: cross-reactive T cells or pre-existing T cell memory that some people have from common cold coronavirus infection. That was basically half of that first Cell paper where we say: ‘we are looking at healthy control people, and we are seeing that some of them have T cells that can recognize this new virus. And that sort of should not happen because nobody has ever had this virus before. So that must mean the T cells were initially recognizing something else, presumably something related. And now they can recognize this virus.’ We published that as quickly as we could, because this potentially has important implications. If some people already have some memory then maybe those people would have some partial immunity to COVID-19 through T cells. Again, it’s not like antibodies, where they would keep you from getting infected, but they might keep you from getting sick, which would be phenomenal.
That work identifying the T cells has been reproduced in Germany, Singapore, a separate lab at La Jolla Institute with samples from the UK and Sweden. The T cells certainly exist. The question is: what do they mean? They might provide you some partial immunity, which would be awesome. They might do nothing. Or they might make you more sick, because they’re really there to recognize something else and now they have a new job. We honestly don’t know because it’s a hard experiment to do. One way to do it is in a vaccine trial where you take a group of people and say: ‘alright, who among this group have cross-reactive T cells’? Let’s say it’s 20 percent of the group. Then you give them the vaccine and say, ‘alright, did something different happen in those 20 percent compared with the other 80 percent?’ The other straightforward way to do this would be to bleed everybody in Brooklyn who hasn’t already been infected with SARS-2, and say ‘alright, we’re going to take those blood samples and keep them and we’re going to wait three months.’ And then at the end of the three months, we say ‘OK, who in Brooklyn got infected’ We’re going to bleed those people again, and of the people who got infected we ask ‘OK, how sick did you get and how does that compare to whether you had any cross-reactive reactive T cell memory?’
AS: Another point to make is that there has been a lot of confusion and people have misinterpreted what we were reporting. Some jump to the conclusion that having a T cell response means we are protected from disease. Having a pre-existing reactivity of immune system should not be interpreted in the other meaning of the word ‘immune’: that you’re Superman and viruses bounce off you and you don’t get infected. You’re not immune to a disease because you have some immune system reactivity. The two things may be linked, but it’s a huge leap of interpretation, that we are not supporting.
MM: What are you looking at now?
SC: The herd immunity thing, which you brought up earlier, has certainly been a pretty big deal in public circles and political circles, which we think has been misinterpreted. We have written an article trying to explain it. Now, it’s been accepted in Nature Review of Immunology and we think it’ll be out in about 10 days. It’s an explanatory piece, it doesn’t have any new scientific data. It’s explaining what the word ‘herd immunity’ actually means and how T cells potentially affect that number. Basically the upshot is: it’s speculated that pre-existing, cross-reactive memory T cells, could help control the virus in some people. That could be a wonderful thing and it might help explain why some people really don’t get sick and some people get really sick. But just because of the way T cells work, there’s no expectation it would actually affect the herd immunity number. Herd immunity is about transmission as opposed to how many people felt sick. If there’s a prospect of T cells doing something positive, it’s going to be reducing disease severity, not preventing infections and cases.
***
Get a digital subscription to The Spectator.
Try a month free, then just $3.99 a month
***
MM: A lot of politicians globally are talking about, in their campaign platforms, the ‘eradication’ or ‘elimination’ of COVID-19. Are those the right terms to use in terms of talking about how to manage a novel coronavirus like SARS-CoV-2?
SC: The simple answer there is, the only virus to ever be eradicated is smallpox. One of the reasons it could be eradicated, actually, was that it had very clear symptoms. Everybody who was infected got these pox. Humans have tried to eradicate other things. And with vaccines have gotten really close.
AS: Like polio. To me it seems premature to raise the possibility of eradicating COVID-19 because we do not have a vaccine that even works, yet. Basically it’s like ‘are we going to be able to eliminate whatever the rodent was in Australia that was creating havoc?’ And we don’t even have a trap yet. Let’s go in steps. Eradicating something is not a one year proposition. In all of these cases, it took years, decades. The problem isn’t to eradicate right now, but to control.
MM: It’s not even a stretch goal ultimately. Right?
SC:I’d say the stretch goal would be for it to be like other diseases that have been fantastically controlled by vaccines, diseases like diphtheria which was quite lethal, down 99 percent; polio, down 99 percent; vaccine examples like that.