Uppsala
The culture of social distancing does strange things to us. A few weeks ago I got an invitation to an offline work dinner, and I can’t remember the last time I had such a sudden rush of joy. Even if life in Sweden over the past two months have been surprisingly normal, the truth is that we all have hunkered down a bit. Many of us have worked from home. The first two weeks, I admit, felt as life in remission — like a sudden gift of time. But then we all sunk into the apathy of having our life on hold. It felt pointless to plan for the future. A reunion with the colleagues became a distant wish. Meeting a work contact for lunch? Surely that’s only something for the privileged few. So getting that invite to a work dinner felt like I had secretly been given the password to attend a Roman bacchanal.
The Swedish economy has finally started to un-Zoom itself. Bicycling lanes in Stockholm now feature the morning pelotons of commuters again. Carmakers like Volvo have opened up their factories and white-collar workers are gradually returning to their offices. Most workplaces have developed their own routines and protocols for COVID-19 safety — and, frankly, most of it is common sense: make it easy for staff to keep good hygiene and avoid having many people showing up at the same place at the same time.
So there’s no hot desking. Those who cannot bike to work are allowed to come in or leave early so they can avoid crowded buses and tubes. Lunch boxes are delivered by restaurants to the workplace. Meeting rooms and common spaces are closed or furnitured around protective acrylic glass. Colleagues that have had coronavirus get additional responsibilities. At the Stockholm accountancy I use, one of the bosses who got infected in early March now manages the afternoon cake trolley. They call him ‘Mr Antibody’ because he doesn’t relish the corporate fitness program as much as the cakes he serve.
It’s common sense attitudes like these that have made foreign observers to take a second look at the ‘Swedish experiment’. We’re no longer just the bad boy of corona — the jumped-up little country that refused to accept lockdown. Yes, we have observed social distancing, but individuals and firms have been allowed to figure out on their own how to practically organize things without having to shut everything down. So the real Swedish experiment has been about ‘behavioral change’: getting individuals to voluntary change their behavior to avoid getting infected or spreading the virus to others. And it has worked.
All this means quite a lot now. Swedes have had 10 weeks of training themselves in how to live together with the virus. ‘Sweden represents a future model if we want to return to a society that we do not have to close’, says the WHO’s Mike Ryan. Most people in Sweden aren’t generally afraid of meeting other people or being in environments where the virus could spread: they manage the risks by keeping a social distance. Polls show that more than 50 percent think they have had coronavirus or that they will get it; only 15 percent think it’s improbable. Perhaps it is this attitude that have prompted so many around the world to think of us as reckless and foolish: we have, in our normalcy, become an ethnographic study object. But all the training we’ve had in sharing the society with coronavirus has taught us that it isn’t dangerous to leave your home or send your kids to school. People don’t have to fearful of living their life in a pretty normal way. Remarkably, seven out of 10 Swedes think the future actually looks bright.
Trusting people that they’ll take advice and change their behavior have also had the desired result. Mobility declined, but not to a level that crushed the economy. The epidemic modeling did not factor in that people would react to a request.

Swedish COVID-19 trends are pointing in the right direction. Fewer ICU beds are now occupied, especially in Stockholm where the number of patients in intensive care has dropped by almost 40 percent since the peak. The daily intake of new intensive care patients is now in the low double digits. The daily death toll flatlined in the second half of April and, mercifully, has since been on a declining trend. And then we have the reproduction rate of the virus — the famous R number that now seems to command much of the British exit strategy. We’ve been warned by Neil Ferguson and others that Sweden’s R number is still in the region of 1.3-1.4 — meaning that the virus still spreads exponentially. However, the Swedish Public Health Agency gives a very different estimate: the R has been below 1 since mid-April or so, and now stands at about 0.85. Britain’s R-number is estimated to be between 0.6 and 1.0 — so if you go by average, we’re in roughly the same place. Sweden got to this level with a far-lower reduction in mobility, so our experience may serve useful to those seeking to measure the relationship between lockdown and the transmission of a virus.

Excess mortality is still the bugbear for foreign observers who want to learn from Sweden. It’s also an issue for Swedes. Even if the time for comparing and making judgments about coronavirus mortality is a few years into the future, it is obvious that Sweden has a big scandal on its hands: it has failed to protect nursing homes against the virus. More than 50 percent of all nursing homes in Stockholm have had infected residents. For the country as a whole, almost 75 percent of all COVID-19 deaths were residents at nursing homes or elderly with home care. Something has gone badly wrong.
What’s going on here? Obviously, the Public Health Agency — along with other agencies — failed to understand the risk that staff could spread the virus in care homes. For a long time, nursing home and home care staff had no access to personal protective equipment (PPE), and once they got advanced equipment, few had been trained in how to use them. Swedish nursing homes also have many residents, and they come there at a very late point in life — so when a virus gets into the nursing home, it can infect many ‘elderly-elderly’ who are frail and have a poor immune system. Add to that failures of centralized medical procurement, for instance, or government complacency in building up capacity to test care workers. It’s no consolation that we share all these problems with other countries. It took us weeks and weeks to fix all these problems, and some of them still haven’t been adequately resolved.
***
Get three months of The Spectator for just $9.99 — plus a Spectator Parker pen
***
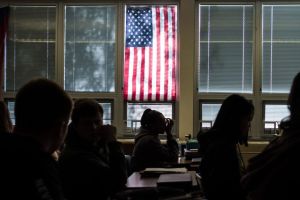
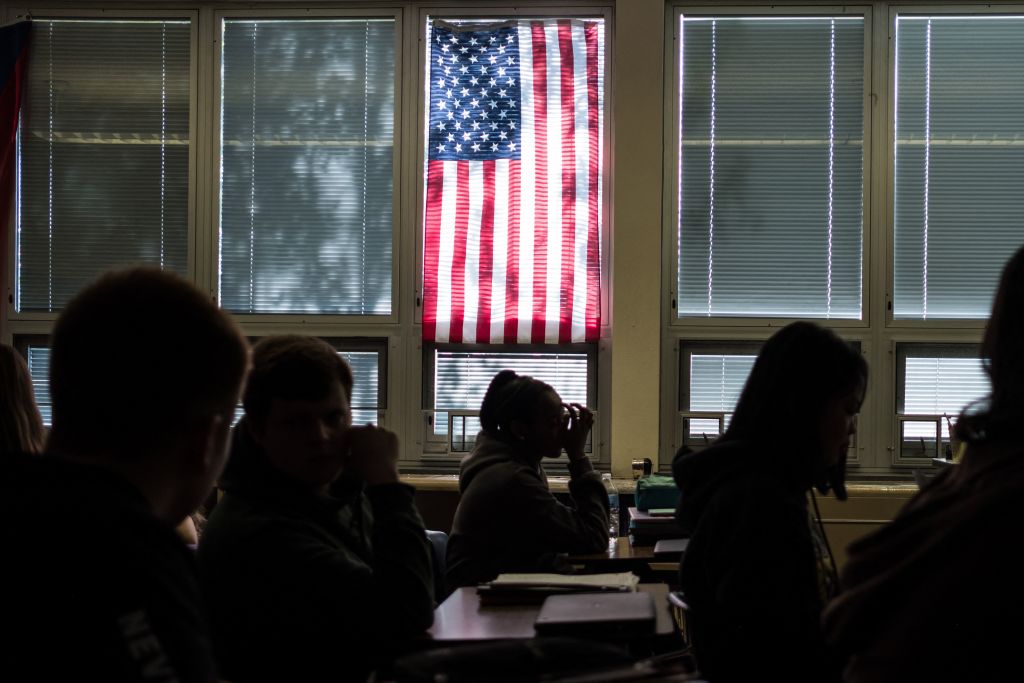
Boris Johnson doesn’t need a warning from Sweden about the risks of care-home deaths: Britain’s experience is actually worse. But he can learn from the Swedish example that people will respond to advice about social distance and change their behavior. Boosting testing capacity is necessary, as is keeping track of the reproduction rate. But at some point Britain needs to take the plunge and encourage people to go about their lives. It’s understandable that many Brits don’t want to end the lockdown and expose themselves to greater risks of getting infected. There is so much that we don’t know about the virus. But confinement is not a good way to manage uncertainty. Just as people with opposing ideas can become political creeps when safe-space culture protects us from them, the world out there gets scary when we shelter in our homes for months.
This article was originally published onThe Spectator’s UK website.