The common horseshoe bat, Rhinolophus affinis, is a feat of biological engineering. The size of a small pear, it spends most of the day hanging upside down in dark, dank caves. To keep itself warm it huddles in tight colonies, wrapping its wings — which can measure up to two inches — around itself like a blanket. Even so, in winter its body temperature can fall as low as 43°F.
Then, two hours before sunset, it emerges to forage for insects using a horseshoe-shaped sonar dish on its nose to find its bearings. But now it has a new problem: flying requires so much energy that its metabolic rate can spike as high as 34 times its resting level, and its core temperature can exceed 104°F, causing cells within its body to break down and release bits of DNA.
Ordinarily, these cell fragments would cause inflammation, but thanks to bats’ weakened immune systems, they don’t. Instead, R. affinis and other species of bats can tolerate a wide range of viruses that in other mammals would trigger aggressive and sometimes deadly immune responses.
That is good news for bats, but potentially very bad news for humans. Bats harbor thousands of viruses, including coronaviruses, any one of which, under the right ecological and epidemiological conditions, could be the spark for the next pandemic.
No one can yet be certain where SARS-CoV-2, the coronavirus that causes COVID-19, originated. But its nearest relative is a coronavirus isolated by Chinese scientists from an R. affinis bat that roosted in a cave in Yunnan, south-west China, in 2013. The virus, dubbed RaTG13, shares 96.2 percent of its genome with SARS-CoV-2. Case closed, you might think.
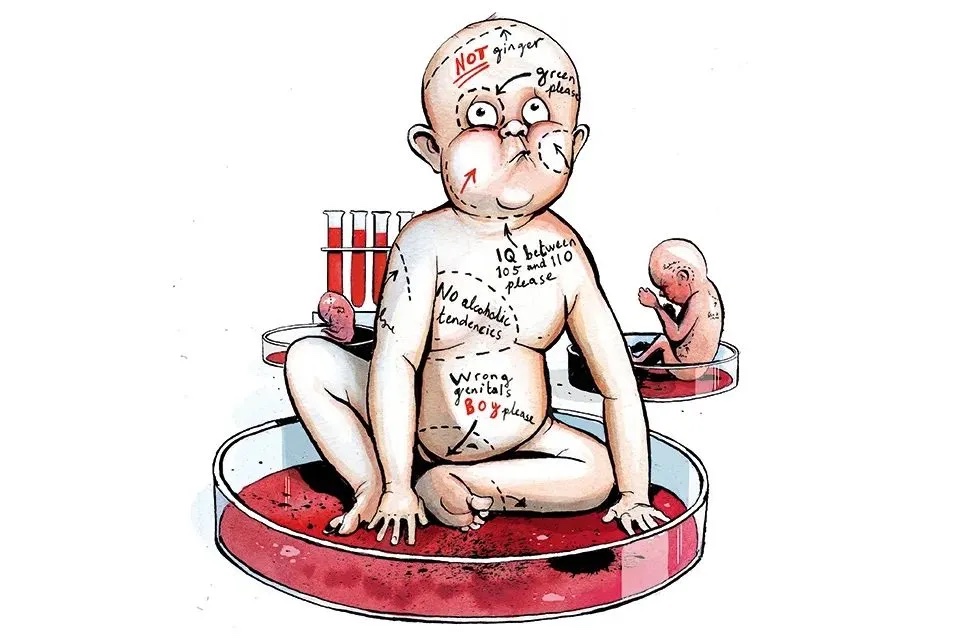
However, the virus is missing a key gene that enables it to attach to cells in the human respiratory tract (interestingly, in the human virus, this section of the gene more closely resembles a virus found in pangolins smuggled to China from Malaysia). In addition, the human virus possesses a unique ‘furin cleavage site’, a sort of molecular can opener that allows the virus to get into host cells. Moreover, Yunnan is 800 miles from Wuhan, where the first human cases of COVID-19 were reported in or near a wild animal market.
That is not to say SARS-CoV-2 did not originate in R. affinis or some other species of horseshoe bat; only that these mutations probably occurred a long time ago — the 3.8 percent genetic divergence with RaTG13 is equivalent to an average of 50 years (and a minimum of 20 years) of evolutionary change — and the particular bat involved has yet to be identified, as has the path of infections which led to the outbreak in Wuhan at the close of last year.
This is hardly surprising when you consider the sheer abundance of bats, which make up a fifth of mammal species on the planet, or the diversity of their ranges. ‘If you go to Malaysia and you sit on the edge of a river with a street lamp nearby, you’ll see bats flitting about all night long eating insects,’ says Peter Daszak, a British-born veterinary ecologist and president of EcoHealth Alliance, a New York-based non-profit that trawls disease hotspots in search of novel bat viruses. ‘They are extremely abundant, extremely diverse, and so are their viruses.’
It is also common to find different species of bats sharing the same roosts. For instance, in Guandong, southern China, horseshoe bats frequently roost alongside fruit-eating Rousettus macrobats. This exposes them to each other’s viruses and makes it more likely they will exchange genetic material.
Once a virus is circulating in bats, all that it takes for it to spill over into humans is for someone to come into contact with feces or fluids from an infected animal. This could happen, for instance, when a local farmer enters a bat cave to collect guano to fertilize his crops or to net a bat for the table. ‘If you’re a poor farmer in south-east Asia and you’ve got a bat cave nearby, it’s free protein,’ explains Daszak. ‘It’s absolutely like fishing in a river in the UK.’
Another key factor is deforestation. Tropical forest edges are a major launch-pad for pandemics. Edges arise as humans build roads or clear forests for timber production and agriculture. Road building, mining and logging camps, and livestock and crop monocultures, such as palm oil, all increase the risk of the spread of animal viruses to humans. In addition, people frequently enter forests to hunt wild game — pangolins, raccoon dogs and palm civets are highly prized in Chinese cuisine and traditional medicine.
But perhaps the most important ecological insight is that spillovers of bat viruses occur all the time. In 2018, EcoHealth Alliance conducted a survey of people living in rural parts of Yunnan and found 3 percent carried antibodies to bat coronaviruses. Extrapolating across the entire range of bats that carry these viruses in south-west China and bordering areas of Myanmar and Laos, Daszak estimates it could mean that ‘right now, every year’ as many as seven million people in the region are being infected with bat coronaviruses. Indeed, Daszak estimates that based on the rate of scientific discovery, there may be as many as 13,000 new coronaviruses out there waiting to be discovered.
But coronaviruses are not the only threat. Bats also carry marburg, nipah and hendra viruses, which have been the cause of human outbreaks in Africa, Malaysia, Bangladesh and Australia. They are also thought to be the reservoir of ebola, which caused a major outbreak in West Africa in 2014-16. When you include viruses harbored by other wild animals, Daszak estimates there may be as many as 1.7 million undiscovered viruses in wildlife. That is an awful lot of pandemic potential.
[special_offer]
Given the clear link between deforestation and virus emergence, one solution would be to reduce dependence on land-intensive monocultures through subsidies and direct forest-protection payments. Another would be tighter regulation of the trade in wild animals, a $75 billion industry in China employing some 14 million people.
The time to act is now. Daszak and his colleagues have identified 335 emerging infectious disease events between 1940 and 2004, with a peak incidence in the 1980s at around the time of the Aids pandemic. Their survey leaves little doubt that these events have been increasing in incidence since the mid-point of the last century.
‘A pandemic such as this one isn’t a once-in-a-lifetime tragedy,’ says Daszak. Whether or not the next pandemic is sparked by a coronavirus or some other animal-origin virus, ‘there will be another one’.