It is counterintuitive but the current spread of COVID may on balance be the least worst thing that could happen now. In the absence of a vaccine, and with no real prospect of eradicating the disease, the virus spreading among younger people, mostly without hitting the vulnerable, is creating immunity that will eventually slow the epidemic. The second wave is real, but it is not like the first. It would be a mistake to tackle it with compulsory lockdowns (even if called ‘circuit breakers’), whether national or local. The cure would be worse than the disease.
If you cannot extinguish an epidemic at the start, the best strategy is for the healthy to get infected first. Lockdowns ensure that the vulnerable and the healthy both get infected with similar probability. School closures, concluded a recent paper in the British Medical Journal, can paradoxically lead to more deaths by prioritizing the protection of the least vulnerable.
In July the World Health Organization said full lockdowns could be ‘the only option’ to prevent resurgence. But last week Dr David Nabarro, a WHO special envoy for COVID-19, told Andrew Neil on Spectator TV that ‘We in the WHO do not advocate lockdowns as the primary means of control of this virus… We really do appeal to all world leaders: stop using lockdown as your primary control method.’
Back in March when the pandemic first poleaxed the West, I argued in these pages that ‘there are no good outcomes from here. Many people will die prematurely. Many will lose their jobs. Many businesses will go under. Many people will suffer bereavement, loneliness and despair, even if they dodge the virus.’ That is still true. There is no course that involves zero suffering. It’s a question of minimizing it.
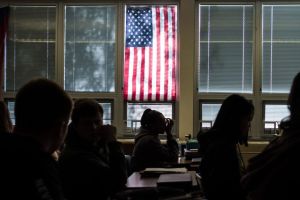
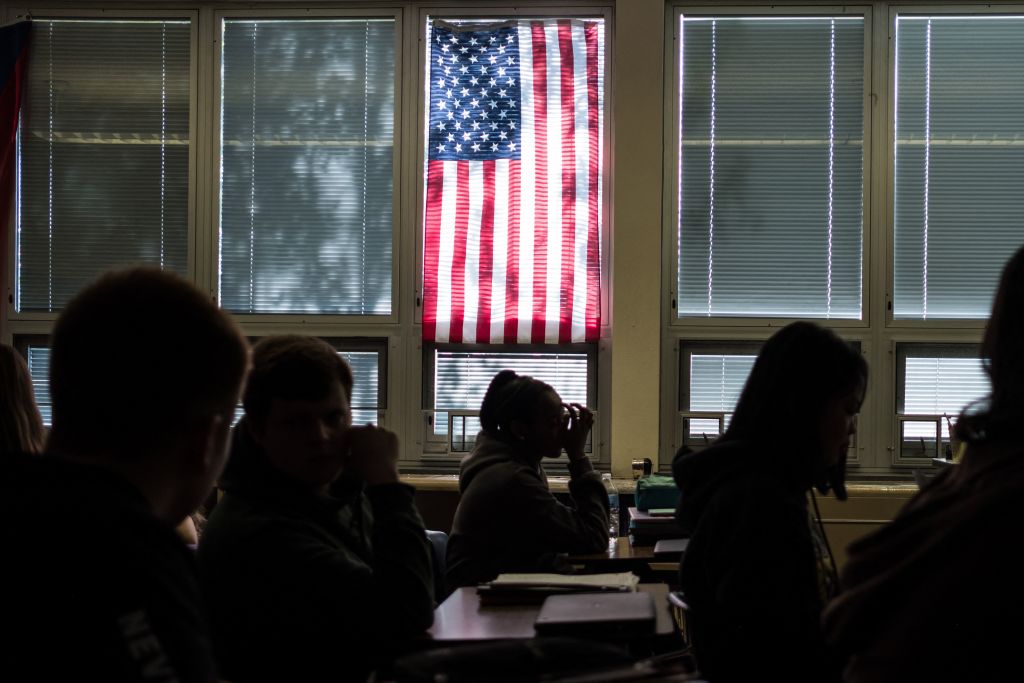
This time, unlike in the spring, the virus has been mostly spreading among students. Places in Britain where more than 25 percent of the population are university students have seven times the positive test rate of the rest of the country. Among students the infection is mostly asymptomatic or mild. As of last week, 70,000 students in the United States had tested positive with just three hospitalizations (one released) and no deaths.
By contrast, the effect of lockdowns on the mental health of young people is huge. Psychologists report that anxiety and depression have sky-rocketed, especially among the young, so that the highest mental impact is being felt among those least likely to die. It’s not COVID that is causing this, but lockdown and recession.
As Professor Karol Sikora puts it: ‘It’s clear that mass testing at universities has uncovered a huge amount of positive results that are largely behind some of the higher numbers. These are already on the way down in some areas. It’s not unreasonable to question whether this has been properly taken into account.’
Consider my home city of Newcastle in northern England. Roughly 50,000 students moved into Newcastle last month. On October 3, Northumbria University announced that there were 770 positive tests among its students, and just 78 of those showed any symptoms at all: that’s 90 percent showing none. In the seven days up to October 5, the Evening Chronicle reports, there were 609 positive tests (I refuse to call them cases) in the city center, Shieldfield and Heaton Park — areas where students live. In Scotswood, a short distance away and where few students also live, there were 16.
It is the ability of this virus to be spread by those not showing symptoms, yet also sometimes to kill, that makes it so hard to control and so dangerous. Back in March the disease was spreading mostly within hospitals and care homes, among highly vulnerable people and their carers. Policy was based on the false assumption that most people would show symptoms, so carers could go from home to home without testing. That was a big mistake, as the medically trained entrepreneur Hugh Osmond kept telling me at the time: many fatal cases of COVID were caught after going into hospital for something else.
Locking down the whole of Britain, schools, pubs, offices and all, did little to prevent that tragedy: health workers were not locked down. But it prevented the growth of natural immunity that happens to some extent with most viruses and thus probably made a second wave inevitable.
At the time I thought it was nonetheless necessary because of the dangerous nature of the virus. As I wrote here in March: ‘The government is now effectively admitting that even if drastic curfews lead to successive waves of the disease, that may be the least worst outcome. It is still a daunting prospect. Successive waves mean successive curfews and successive body blows to the economy. If we clamp down hard now and the infection rate drops, then we might be able, slowly and cautiously, to restart the economy in the summer but have to clamp down again when the virus resurges. Each time we do this, it will be more painful.’
Yet Sweden shows that the second wave could have been largely avoided. At the end of March, on the very weekend Derbyshire police tried to shame solitary hikers in the Peak District back indoors with drones and snide tweets, the Guardian described how ‘Malmo’s café terraces do a brisk trade. On the beach and surrounding parkland at Sibbarp there were picnics and barbecues this weekend; the adjoining skate park and playground were rammed.’ The New York Times called Sweden a ‘pariah state’. The Sun headline read: ‘Sweden’s refusal to enter coronavirus lockdown leaving schools and pubs open “will lead to catastrophe”, doctors warn.’
[special_offer]
It did not. Sweden, a slightly more urbanized society than Britain, suffered almost as high a death rate in the first wave — it likewise failed to protect care homes — but is seeing almost no second wave. More to the point, its economy is in much better shape and therefore so are people’s lives. It ran a budget surplus in August and its economy is forecast to shrink 3.3 percent this year compared with 5.8 percent for the UK. Had we protected hospitals and care homes while keeping schools and pubs open, the chances are we too would be much better off.
Or look at London, where just 34 people died of COVID in the first week of October, compared with more than 1,000 a week in early April. There isn’t much of a second wave there, despite — or because of — demonstrations and crowded tube trains during the summer. This is probably because London’s first wave was already well advanced when lockdown started. Given widespread immune responses to the four kinds of corona-caused common colds, and the skewed pattern of viral infection, whereby a few super-spreaders cause most of the new cases, it looks increasingly as if the virus is already finding it harder to spread in the capital this time round.
The alternative to lockdown is not ‘letting the virus rip’, as Boris Johnson puts it. The Great Barrington Declaration, signed by over 20,000 doctors and medical scientists (but disgracefully censored by Google’s search engine), calls for focused protection: help the elderly and vulnerable stay at home, but let the young and invulnerable go out and achieve immunity for us all, while earning a living. The extraordinary truth is that a student catching COVID might be saving Grandma’s life rather than threatening it.
This article was originally published in The Spectator’s UK magazine. Subscribe to the US edition here.