Should we, or should we not be compelled to wear face masks during a virus epidemic? It sounds a simple enough question. Indeed the answer seems so obvious to many, including the Mayor of London, Sadiq Khan, that they are questioning why this measure is not already mandatory. Surgeons wear them; they filter the air we breathe; viruses are in the air; let’s get everybody wearing them. Other countries have, so they must be helpful. It seems so straightforward.
Unfortunately it’s not as simple as that, and the obvious becomes less obvious the more you look at it. ‘Following the science’ often feels like chasing a receding target, which throws up more questions than it answers, before disappearing over the horizon, leaving those responsible with a political, judgment-based decision to make. The reasons this happens so often involve both imagination failure when faced with a complex problem, and the limitations of science. But it’s important that we all have an idea of how far the science can take us, so we can think clearly about political decisions that may limit our freedoms or compel certain actions. If we are to be told that decisions are scientifically justified, we need a discussion about that scientific basis, not just be told to take our medicine.
To think about this in relation to face masks, you first need to have a handle on just how small viruses are. A human hair is about a 10th of a millimeter thick. A typical bacterium (such as the human pathogens E. coli or S. aureus) comes in at about one thousandth of a millimeter, so you could line a hundred up across the width of a hair. A coronavirus particle is about 10 times smaller still, so a thousand would fit across a hair. This extreme smallness was instrumental in the discovery of viruses in the 19th century: they were the infective agents, left in solutions that had been passed through ‘ultrafilters’ which had removed all other known pathogens.
So to filter out viruses effectively you need a filter with a very fine mesh indeed, even assuming that all the air goes through the filter. And you need to think about which way the air is going: breathing in (the idea being to protect you) or breathing out (ostensibly to protect others if you have the virus).
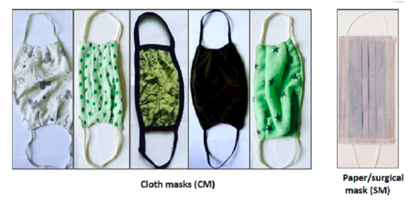
A recent study looked microscopically at pore sizes in low-cost face masks of the types common in developing countries such as Nepal, made from various cloth materials. Here’s a sample they showed in the study.
They found pore sizes of roughly one to five human hair widths — the pore sizes got slightly bigger after washing. So in relation to viruses, these masks are doing little, except possibly reassuring their wearers.
The surgical-type face masks, more likely to be used in developed countries, are a bit better. They have pores typically three times larger than the virus particles, rather than the one to five thousand times larger for the cloth masks. Better, but still not good enough to filter out viruses. A laboratory study by the Health and Safety Executive looking at influenza virus, which is a similar size to coronavirus, found live virus in the air behind all surgical masks tested. They tested masks on a human volunteer using an ‘inert aerosol challenge’ (a simulated sneeze), and on a breathing dummy head using a live virus aerosol challenge. The numbers of particles were reduced by a factor of two for the human volunteer, and six for the dummy head; probably not very effective in reducing infection when infective aerosols — the droplets emitted from someone’s cough or sneeze, or even during talking — may contain hundreds of thousands, or millions, of tiny particles.
But the thing to understand about this science is that those breathing-in factors represent the very best that could possibly be achieved. The masks were adjusted ‘in order to obtain the best fit possible’ and ‘the test subject was asked to remain still during the test’. Obviously, the dummy head was completely still — in real life this just doesn’t apply. Masks don’t fit snugly, people move all the time, the mask material gets damp and air gets around the side. What if you sneeze, cough, burp, sigh, yawn, or readjust the mask? What if you touch your face to ease an itch caused by the mask? More air gets round the side. The reduction factors in actual use, over a day rather than half a dozen measurements, are likely to be much nearer 1 — no protection at all — than those measured in the lab.
What does this mean in terms of protecting yourself when you breathe in? It seems very much along the lines of wear one if you want to, but don’t expect it to stop you getting the virus from aerosols – which are likely to have an important role in viral transmission, especially in crowded or busy environments. In other tests, masks are better at filtering out large droplets. But of course the real-life caveats of moving and breathing around the side of the mask also apply, and large droplets may settle on your skin, hair, and clothes, as well as the outside of the mask, and may get into the air when you take off your mask and coat at home, rub your face and put your hand through your hair after a hard day’s work. The mask may protect you a bit, but it may well not.
What about protecting others? Surgeons wear masks mainly to protect their patients from particulate and potentially infective matter falling out of their noses, mouths, mustaches and beards into a patient’s open. We’re talking about big particles here (human hair width) and bacterial infections, not viruses. Even for this situation, which is universally observed, it is surprisingly difficult to generate watertight scientific data about the effectiveness of surgical masks in preventing bacterial infections. For viral infections there is little data, but again, the pores allow viruses through and much of the air you breathe out goes around the side. When a person is infectious with a virus it is estimated that they may shed one hundred billion virus particles a day — that works out at about 10 million per breath. A mask won’t stop you putting these particles into the air around you. In fact, with a damp mask you’ll be blowing aerosols and larger particles sideways, directly at your socially distanced colleagues six feet away. And if wearing a mask tempts you to feel that you’re not going to infect anyone else, you may also be less likely to observe the six-feet rule. So does wearing a mask protect others if you’re infectious? There’s little direct evidence to say that it does, and quite a lot of straightforward reasoning to suggest it doesn’t.
As you might imagine, you can find an awful lot more detail on all this. A recent, non-peer-reviewed review article concludes with a call for widespread mask use, including regulatory enforcement. But the evidence it presents seems very weak for such a strong call, and conflates laboratory, clinical and community studies. There are mask filtration studies; papers describing small, uncontrolled situations, many of which have heavily qualified conclusions (but nevertheless call for widespread measures on the basis of their slim evidence); speculative sociological studies often based in Asia; and ubiquitous modeling which appears to support the conclusions, but is based on non-real-world assumptions about mask ‘efficacy’ and mask ‘adherence’. A multiplication of inconclusive studies does not enhance the evidence base.
***
Get three months’ free access to The Spectator USA website —
then just $3.99/month. Subscribe here
***
The point is: does any of what is out there add up to a watertight case for compelling people to wear masks in public or at work (outside a healthcare setting)? The threshold for compulsion must surely be higher than ‘maybe’ and ‘perhaps’. But if it really is the case that the threshold for regulatory compulsion is being approached, it should be a simple matter for our scientific advisers to present it to us and allow time for it to be critically discussed in relation to a real-world setting, before government imposes measures upon us all.
That other countries may have taken action says things about those countries’ attitudes to open scrutiny of evidence-based decision-making, and their populations’ attitudes to compliance and compulsion. It says nothing about the validity of the measures. Coronavirus is not a reason for us to accept arbitrary impositions or abandon our traditions of rational discourse. The West’s record in these matters is one of our great strengths — its preservation allows us to deal better with crises, especially crises like coronavirus, where there is much more to consider than just the virus itself.
This article was originally published in The Spectator’s UK website.

























