Trust in the public healthcare system declined among Americans during the Covid-19 pandemic. It’s no wonder: public health bureaucrats pushed for various insane policies that ran counter to common sense, admitted to deceiving the American people and worked to shutter debate surrounding the national and global coronavirus response. But instead of doing everything they can to restore trust in the system (and prove that they’re still deserving of it), government officials and medical associations have continued to politicize the healthcare field, sowing discord between patients and their doctors.
A consistent theme throughout the pandemic was that while Americans were less likely to trust the medical establishment, they mostly liked their personal doctors. But some new policies proposed and enacted by left-wing activists and politicians threaten the doctor-patient relationship.
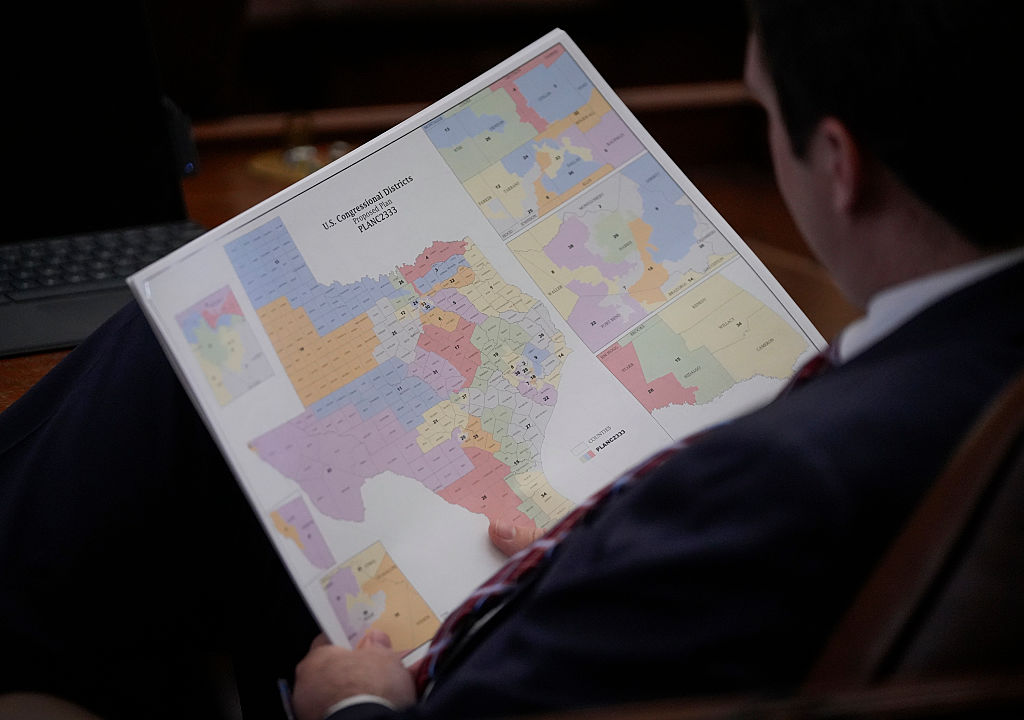
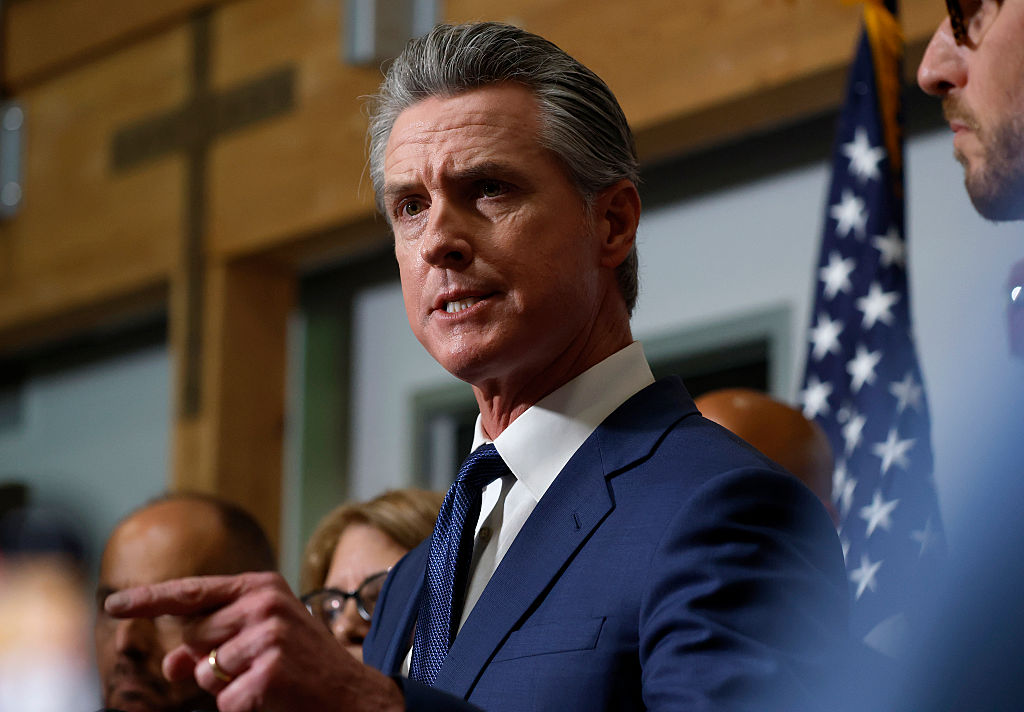
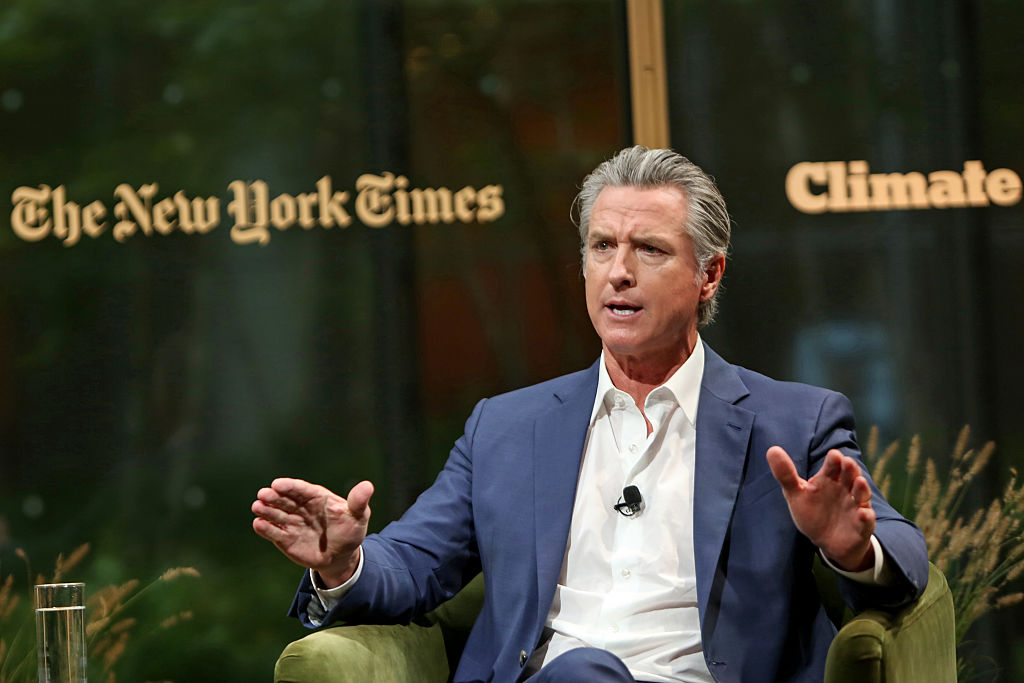
Lawmakers in California passed legislation in 2019 that requires all continuing medical education courses to include implicit bias training. Doctors in California need to complete fifty hours of continuing medical education every two years. AB 241, signed in October 2019 by Governor Gavin Newsom, says that these courses must include “examples of how implicit bias affects perceptions and treatment decisions of physicians and surgeons, leading to disparities in health outcomes,” or “strategies to address how unintended biases in decision making may contribute to healthcare disparities by shaping behavior and producing differences in medical treatment along lines of race, ethnicity, gender identity, sexual orientation, age, socioeconomic status or other characteristics,” or a combination of both.
Sign up here to receive the Culture Shock newsletter in your inbox on Wednesdays.
Activists have long argued that doctors carry implicit bias — or unconscious prejudices — against patients of certain races or genders. They point to studies suggesting women in pain are more likely to be underdiagnosed and undertreated, for example, or that black women are more likely to die after being diagnosed with breast cancer. However, the most popular test “proving” that people carry unconscious bias has serious methodological problems. Plus, disparate healthcare outcomes among different racial and gender groups may have other, more innocent explanations; women may be less assertive about their pain levels, for instance, and patients of color may be slower to seek care due to historical issues with the healthcare system.
There is also no evidence that implicit bias training works. Research finds that such training rarely results in sustained changes in attitudes or behavior — and worse, may have the opposite of the intended effect. Trainees who are accused of harboring bias may become angry, frustrated or resentful in response.
Another unintended side effect of insisting that doctors are racist and in need of training to root out their prejudices is that it could induce hesitancy among patients to seek care or to distrust the opinions of their doctors. Patients who are repeatedly told they have to watch out for implicit bias are already entering the doctor-patient relationship with suspicion that their doctors might be intentionally or unintentionally harming them.
To that end, a group of doctors represented by the Pacific Legal Foundation filed a lawsuit seeking a permanent injunction against AB 241. Dr. Marilyn Singleton, a visiting fellow of the Do No Harm organization and anesthesiologist, and Dr. Azedah Khatibi, an ophthalmologist, who both teach continuing medical education courses in California, are challenging the legislation alongside Do No Harm, a national association of medical professionals based in Virginia.
“The implicit bias requirement promotes the inaccurate belief that white individuals are naturally racist,” said Dr. Singleton. “This message can be detrimental to medical professionals and their patients as it creates an atmosphere of suspicion and animosity, which goes against the fundamental principle of doing no harm.”
The Pacific Legal Foundation will argue that the implicit bias training requirement infringes on the free speech rights of doctors who teach continuing medical education courses. In order to legally compel speech, California must prove that there is both a compelling government interest at stake and that the law is narrowly tailored to achieve its goals.
Caleb Trotter, an attorney on the case, argues that the implicit bias requirement fails on both counts.
“The government here is going to have to show evidence that requiring implicit bias instruction addresses some kind of compelling interest they may have. Maybe they’ll say things like, ‘This is addressing discrimination in healthcare.’ They’re going to need to have evidence to support that,” Trotter told The Spectator. On the question of narrow tailoring, the government will have to show that alternatives to addressing alleged implicit bias in the medical profession were insufficient in addressing the problem.
“Were there other ways that the government could have addressed the problem that are less restrictive or less compulsive in regard to speech?” Trotter continued. “They could have done what the legal profession does, which is just require physicians to take one course.”
Dr. Khatibi, who immigrated to the United States from Iran, believes that implicit bias exists and needs to be addressed, but takes issue with the implications California’s law has on speech.
“I deeply believe that it’s unconstitutional for the government to compel the speech of individuals. And so that’s why when the opportunity came for me to fight it, I decided to join the lawsuit,” Khatibi told The Spectator. “I was born in a country, Iran, where there is no freedom of speech, and it was quickly taken away. I see how people suffer and I see how the spirit is pushed down when people are not allowed to say what they believe.”
Freedom of speech is especially important in the medical community because vigorous debate allows doctors to determine what is the best care for their patients. Insisting there is only one correct way of thinking, as the California implicit bias law supposes, may lead to a lack of progress in the medical field.
“Do you want the collective of medicine to be under the shadow of coercion? Do you want the collective of medical thought and action to be not free, not where doctors are afraid to speak out? I think it’s important to protect the free speech of doctors at all costs,” Dr. Khatibi said.
Forcing implicit bias training into every continuing medical education course can also take away from the time allotted for doctors to learn tangible things to help their patients. Doctors who take continuing medical education courses may be looking to brush up on preexisting knowledge, learn new skills or otherwise specialize within their field.
“Discussion of implicit bias may or may not be relevant to [a course] topic. If it’s a day-long conference and you have fifteen minutes to impart your knowledge to the audience, it can be very frustrating and inefficient to not be able to talk about the things that you want to teach because you have this additional requirement,” Dr. Khatibi explained. ” And it ignores the other serious issues that create disparities like socioeconomic status, like access issues. We need to have discussions of these as well. And we don’t have them.”
AB 241 is emblematic of a wider problem in the medical industry wherein politicians and activists determine the “correct” treatment options for patients and reject debate among doctors. For example, LGBTQ advocacy groups have pushed medical associations to adopt puberty blockers and hormone therapies as the proper course of treatment for youth suffering from gender dysphoria, despite a lack of evidence that such medicines actually improve mental health outcomes. The Human Rights Campaign has suggested doctors “revise client forms” to match their transgender identity as opposed to their biological sex. According to the New England Journal of Medicine, a woman lost her baby in 2019 because she presented as a man and doctors failed to diagnose her pregnancy.
Dr. Jeffrey Barrows, senior vice president of bioethics and public policy for the Christian Medical and Dental Associations (CMDA), told the Epoch Times that one of his group’s members was fired for writing the biological sex of a transgender person on a medical form.
Barrows said it is “insanity” to introduce such confusion into potentially life-or-death medical decisions.
Understanding differences between groups can be helpful in a medical context. Women, for example, often present different symptoms than men when experiencing heart attacks. But it’s also important that doctors have the opportunity to approach their patients as individuals with unique needs so that they can provide them the best care possible. The increased activist involvement in medicine threatens to take away the special doctor-patient relationship in favor of toxic and divisive identity politics.
Sign up here to receive the Culture Shock newsletter in your inbox on Wednesdays.