Language about insulin is supposed to be one of the bigger selling points of the Build Back Better Act. Democrats say prices would be capped at $35, which is true from a certain point of view. Insulin co-pay prices get capped at $35 — starting in 2023 — for Medicare Part D and Medicare Advantage plans. Individual and private insurers face different rules, however, only having to charge $35 for either a vial or a pen. They can also pick one kind of insulin to cover.
Insulin price controls are a hot topic right now for good reason. Over the last twenty-three years, Humalog brand insulin has gone from $21 a vial to $275. The generic version of insulin called Semglee costs almost the same. Rebates exist but it’s still a hefty price tag given that generics are typically 85 percent cheaper than brand-name drugs.
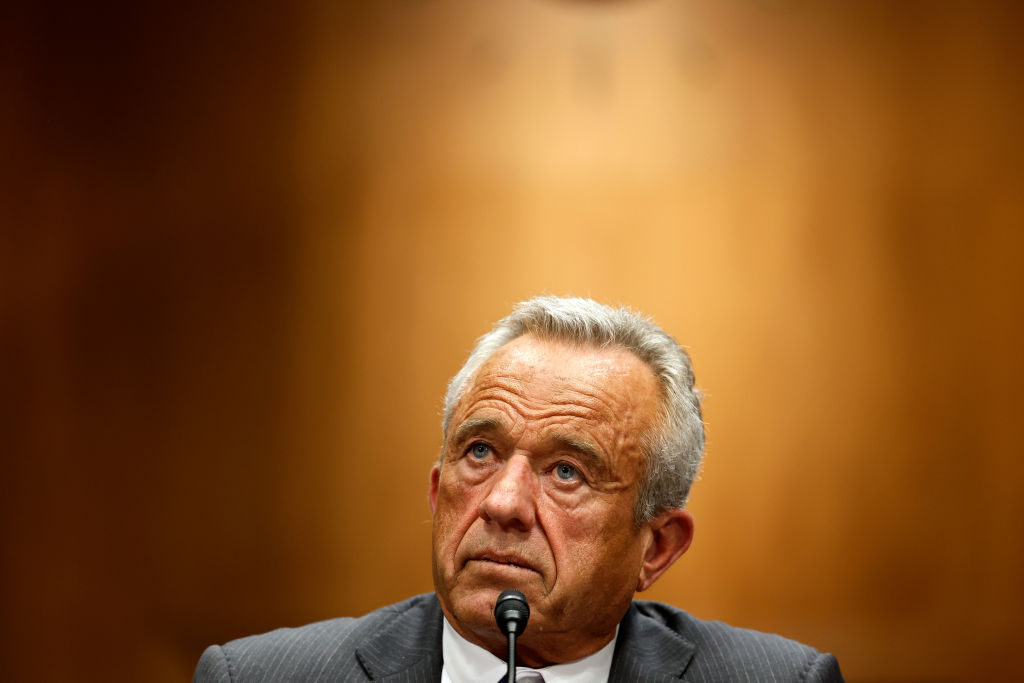
Democratic senator Ron Wyden and Republican senator Chuck Grassley blame pharmacy benefit managers for skyrocketing insulin prices. PBMs like OptumRX and CVS Caremark negotiate drug prices for pharmacies, yet Wyden and Grassley wrote in January that they suspect these talks do little to reduce insulin costs. The pair specifically blamed PBMs for pitting drug makers “against each other” in hopes of getting more rebates and more cash via administrative sales.
Their investigation also discovered that the three American manufacturers of insulin tended to raise prices when one of their domestic competitors did the same. It appears their motives were more to keep PBMs happy than to pad their own pockets with cash.
Although bipartisan agreement clearly exists on insulin prices, Democrats and progressives don’t think Build Back Better goes far enough. The New Republic argued last month that there needed to be a full price control on insulin, citing insulin rationing. Senator Bernie Sanders campaigned on breaking up the pharmaceutical companies and capping medication costs at $200 a year. Wyden and Grassley have been working together on insulin price legislation since 2019 (Grassley does not support Build Back Better’s drug language). Republicans, including Mississippi attorney general Lynn Fitch, have sued insulin manufacturers and accused them of inflated pricing.
Insulin manufacturers deserve a lot of criticism for rising prices. A House Oversight Committee report from last week accused companies of manipulating the US patent formula with minor tweaks to their product. Pfizer has kept a stranglehold on the American market for a fibromyalgia drug through a pediatric marketing exclusive deal with the FDA. Pharmaceutical companies have raked in cash by taking advantage of Medicare Part D. All have figured out how to game the system.
Here’s where Build Back Better and other drug price control advocates ignore the biggest issue: government involvement created the very system that drug companies figured out how to exploit. The Food and Drug Administration’s drug approval process takes ten years (!) despite the FDA’s ten-month goal for Standard Review. There’s no incentive for new drug makers to get into the market if they know it takes this long for approval.
Let’s not forget the FDA’s requirement that diabetics get insulin prescriptions. Mexico and Canada have no such government mandate; hence the rise in (technically illegal) insulin tourism by Americans.
Those who worry that getting rid of the prescription requirement would result in insulin overdoses (or underdoses) forget several things. First, it would be ill-advised for diabetes patients not to consult with a doctor before learning what insulin dose they need. Plenty of guides exist on how much and when to change insulin dose levels, plus patients still need to check their blood sugar levels before making any sort of insulin injection. There’s also nothing stopping pharmacies from requiring a prescription or other documentation for insulin before selling it to a customer.
Another problem regards insulin purchases. The FDA bans bulk buying, meaning insulin purchases are limited to monthly or every three months. This despite a lifespan of a year on refrigerated unopened insulin and a twenty-eight-day lifespan on opened insulin. The hoop remains just one reason why the insulin black market exists, and prices remain high.
Build Back Better Act and drug price control advocates wrongly believe that prices will drop if federal negotiations take place with companies. Yet the House Oversight Committee admitted that Medicare negotiators lost $25 billion in savings during talks with pharmaceutical reps. There’s no incentive to hire better negotiators if insulin users only worry about a $35 capped charge.
As for those who point to Canadian and Mexican price negotiation systems, they forget that both focus on patented drugs and not generics. Mexico’s price negotiation framework is voluntary in certain cases. Canada’s price negotiations also involve what pharmacies pay for drugs, not what consumers pay. This is massively different from what politicians in Washington are suggesting.
The co-pay cap plan fails because it pushes costs down the line onto other generations of Americans. It props up a failing system not through meaningful reform but minor tweaks when outlying problems arise. The real solution involves undoing most of the regulations and rules and giving more power to consumers to get the life-saving insulin they need.